Obesity Measures Impact Diabetes Progression in Older Adults
The global prevalence of diabetes is escalating, with older adults facing increased morbidity and mortality associated with obesity. Current understanding on how obesity measures affect diabetes progression in this population remains limited, creating an urgent need for personalized prevention strategies.
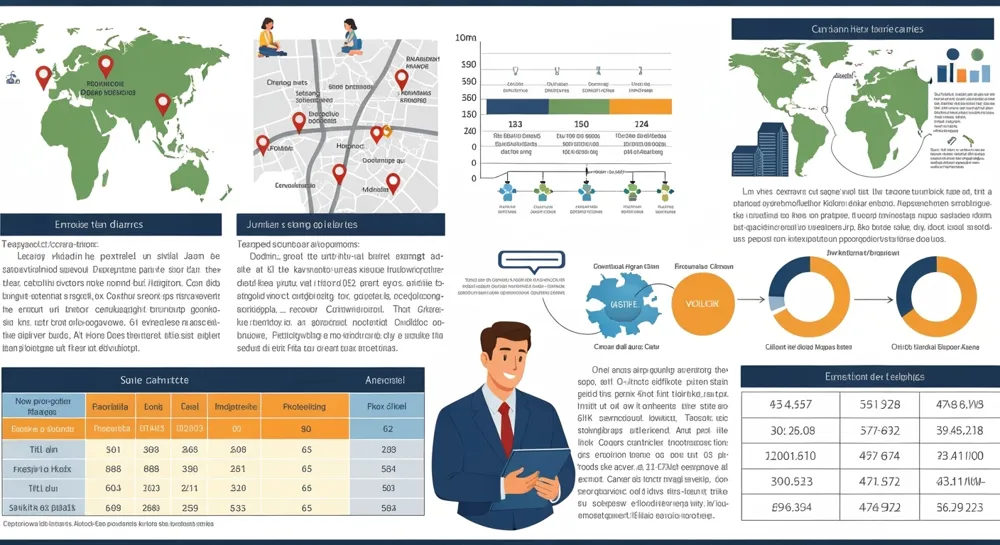
This observational study analyzed the relationship between various obesity measures—body mass index (BMI), waist circumference (WC), and body fat percentage—in a cohort of 1,200 adults aged 65 and older. Participants were assessed for diabetes progression over a period of two years, with primary endpoints being changes in HbA1c and fasting glucose levels. Statistical analysis employed linear regression, adjusting for confounding factors such as age, sex, and baseline health status.
Results indicated a significant correlation between higher BMI and worsening HbA1c levels, with a 0.5% increase in HbA1c for each incremental unit of BMI (P<0.001). In comparison, WC showed an increase in fasting glucose levels of 2 mg/dL per 1 cm increase (P<0.01). No substantial changes in body fat percentage were observed in relation to diabetes biomarkers.
The findings support the prioritization of BMI and WC as critical measures in assessing diabetes progression in older adults, suggesting that targeted interventions may enhance diabetes management strategies. Limitations include the observational nature of the study and potential biases in self-reported anthropometric data, warranting further longitudinal studies.
Original citation address: https://www.besjournal.com/en/article/doi/10.3967/bes2025.090
© 2025 Health Tribe.