Understanding Renal Artery Stenosis and Hypertension Risks
Author: Ji Yu, Attending Physician in the Vascular Surgery Department at the National Emergency Medical Research Center, Emergency General Hospital. Reviewer: Zhang Jun, Chief Physician of the Vascular Surgery Department at the National Emergency Medical Research Center, Emergency General Hospital.
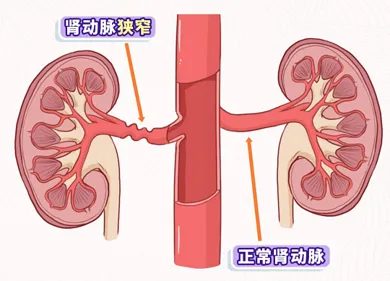
Understanding Renal Artery Stenosis and Hypertension Risks Renal artery stenosis and hypertension worsen each other; early screening is vital for effective treatment and lifestyle management. Keywords: ['Hypertension', 'Kidney health'] Have you ever encountered a situation where your blood pressure remains high despite taking several medications? At this point, you might need to be alert to a possible issue—renal artery stenosis. Hypertension and renal artery stenosis often do not exist in isolation; they can exacerbate each other, creating a worsening cycle. Understanding this cycle is crucial for early detection and treatment. Why does renal ischemia lead to an increase in blood pressure? The kidneys are not only organs for detoxification but also serve as one of the key regulators of blood pressure. When the renal arteries narrow and blood flow decreases, the kidneys may mistakenly perceive that the overall blood pressure is too low. In response, they activate an emergency mechanism known as the renin-angiotensin-aldosterone system (RAAS): the activation signal is renal ischemia, prompting the release of a large amount of renin. 1. Chain reaction: Renin undergoes a series of changes in the body, ultimately forming a potent vasoconstrictor substance—angiotensin II—which also stimulates the secretion of aldosterone. 2. Blood pressure surge: Angiotensin II causes the blood vessels throughout the body to constrict; aldosterone prompts the body to retain more water and salt, resulting in increased blood volume. Together, these factors lead to a sustained and stubborn rise in blood pressure. This condition is known as renal vascular hypertension. What is different about this type of hypertension? Hypertension caused by renal artery stenosis often has the following characteristics, which remind us to investigate promptly: - Particularly stubborn: Blood pressure (especially the diastolic) is very high, and it is difficult to manage even with several kinds of antihypertensive medications. The age of onset is polarized: it is commonly seen in young people (often related to giant cell arteritis and fibromuscular dysplasia) and older individuals (often associated with atherosclerosis). - Accompanied by other signals: Some patients may hear vascular murmurs in their abdomen; some may experience unexplained declines in kidney function; and a very small number may suddenly experience hypertensive crises or pulmonary edema. The course of the illness changes rapidly: hypertension, which was previously well-controlled, suddenly worsens, or new-onset hypertension progresses quickly. — Vicious Cycle: Hypertension Harms the Kidneys. The frightening aspect of this cycle is that hypertension is not only a consequence but can also worsen the condition. Prolonged hypertension can directly damage blood vessels, particularly by: Worsening Narrowing: The high-pressure blood flow impacts the vessel walls, accelerating atherosclerosis, which may lead to the renal artery becoming increasingly narrowed. Directly Harming the Kidneys: Hypertension causes hardening of small blood vessels within the kidneys, exacerbating ischemia and potentially gradually progressing to renal insufficiency or even kidney failure. Affecting the Whole Body: This stubborn hypertension also significantly increases the risk of damage to organs such as the heart and brain. Thus, a closed-loop is formed: renal artery stenosis → activation of RAAS → resistant hypertension → exacerbation of vascular damage and renal ischemia → further deterioration of stenosis and kidney function. How to break the cycle? Once renal artery stenosis is suspected, timely diagnosis and treatment are crucial. Who needs to be screened? Not all patients with high blood pressure require testing, but if your high blood pressure shows the special signals mentioned above, you should be cautious. Common tests include: - Doppler ultrasound of the renal arteries: non-invasive, convenient, and can be used as an initial screening method. - CTA or MRA: Provides clearer insights to help clarify the degree of narrowing. - Renal artery angiography: the gold standard for diagnosis, especially used when preparing for interventional treatment. Treatment: The dual-target approach aims not only to lower blood pressure but also to address vascular stenosis and interrupt the vicious cycle. Vascular recanalization (revascularization) can be performed on eligible patients using balloon dilation or stent implantation to widen narrowed blood vessels and restore blood flow to the kidneys. Early intervention may even hold the promise of curing hypertension or significantly improving it. - Scientific Medication: If there is unilateral renal artery stenosis, the doctor may use pril or sartan medications (RAAS inhibitors), which can target critical points for lowering blood pressure. However, treatment should start with a low dose and require close monitoring of kidney function. Please pay special attention: If both renal arteries are narrowed, or if there is only one kidney and the renal artery is narrowed, the aforementioned medications should be avoided to prevent kidney failure. At the same time, it is important to control blood lipids and blood sugar, and to strictly refrain from smoking. - Lifestyle Management: Make it a habit to measure blood pressure daily and regularly check kidney function (such as routine urine tests and blood creatinine levels). Maintain a diet that is low in salt and fat, and light in nature. Engage in appropriate exercise, control body weight, and avoid strenuous activities. Renal artery stenosis and hypertension are like a pair of mutually harmful partners. In the face of persistent hypertension, being more vigilant about the renal arteries could lead to an earlier identification of the underlying cause. Through timely screening and clear diagnosis, combined with vascular intervention, medication treatment, and lifestyle adjustments, it is entirely possible to break this vicious cycle and protect your blood pressure and kidneys. If your high blood pressure exhibits the characteristics mentioned in the text, it is advised to promptly consult with a cardiology, nephrology, or vascular surgery specialist for a professional assessment.
© 2025 Health Tribe.


