Preventing and Treating Lower Limb Superficial Venous Varicosity

Author: Zhi Yanru, Chief Nurse at the First Affiliated Hospital of Naval Medical University. Reviewer: Li Haiyan, Deputy Chief Nurse at the First Affiliated Hospital of Naval Medical University. Introduction: Varicose veins cause leg discomfort and venous dilation. Prevention includes exercise, weight management, and improved posture. Keywords: ["Disease Prevention", "Health Management"]. Title: Preventing and Treating Lower Limb Superficial Venous Varicosity.
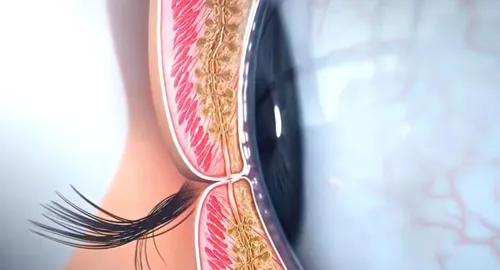
What is "earthworm leg"? The appearance of "little worms" in the legs may indicate superficial venous varicosity in the lower limbs. This condition is primarily characterized by the dilation and degeneration of the venous walls, leading to irregular bulging and twisting. Due to their coiled shape resembling small worms, it is commonly referred to as "worm legs." Why do varicose veins occur in the legs? Varicose veins are primarily caused by weakened venous walls, insufficient closure of venous valves, and increased pressure within the veins. In the venous system of the human legs, numerous venous valves function like one-way valves, facilitating the return of blood from the peripheries back to the heart while preventing backward flow. However, as these one-way valves age or become dysfunctional, their ability to close properly diminishes. This leads to blood pooling in the calves, increased pressure within the veins, and ultimately the twisting and dilation characteristic of varicose veins. In addition to bulging veins, what other symptoms might accompany varicose veins? (1) There is significant dilation of the twisted blood vessels, and noticeable "little worms" on the legs may be seen. (2) Discomfort and soreness in the legs. With the deformation of the venous vessels and potential vascular inflammation, symptoms such as edema and skin itching may arise. Nutritional changes in the skin of the ankle, including eczema, pigmentation, and scaling, if not addressed promptly, can lead to "old leg ulcers". Blood stagnation can also predispose to deep vein thrombosis in the lower limbs, resulting in swelling and pain. If a thrombus dislodges, it could cause a pulmonary embolism, leading to breathing difficulties, chest pain, and potentially fatal outcomes. Common groups prone to lower extremity superficial venous varicosities include obese individuals, pregnant women, those with a family history of varicose veins, and individuals with occupations requiring prolonged standing or sitting, such as nurses, teachers, and retail workers. Additionally, older adults face increased risk due to age-related changes in the veins. Prolonged standing, heavy physical labor, pregnancy, obesity, and habitual constipation are all significant risk factors for varicose veins. Hence, populations such as teachers, healthcare workers, pregnant women, chefs, and office workers tend to be more susceptible to this condition. Extended standing exerts substantial pressure on lower limb veins, gradually degrading the function of venous valves and leading to deformation of the superficial veins, resulting in "spider veins." Furthermore, certain behavioral habits, such as prolonged high heel wear, crossing legs, or sitting with legs folded, may contribute to the development of varicose veins, highlighting the importance of being mindful of these habits in daily life. Preventing superficial venous varicosities in the lower limbs is essential. What preventive measures can be taken? Avoid standing or sitting for long periods and refrain from carrying heavy loads continuously. If work constraints limit movement, engage in simple actions during breaks, such as standing on tiptoes or lifting your legs, to promote venous return. Maintain regular exercise, selecting suitable activities based on personal preferences to enhance blood circulation and mitigate venous pressure. (3) Control your weight; obesity increases the burden on lower limb veins, elevating disease risk. After a day's work, if legs feel sore and swollen, elevating them with a soft pillow is beneficial. Wear flats more often and minimize the use of high heels; if necessary, choose lower wedge heels. Sitting in positions such as crossing legs or sitting cross-legged can compress veins in the popliteal fossa, hindering blood return. Is surgery necessary for already developed superficial venous varicosities? Varicose veins do not necessarily necessitate surgical intervention. The need for surgery depends on various factors, including the severity of the condition, symptoms, the patient’s quality of life, and personal preferences. For those with mild or no symptoms, non-surgical treatments are usually adequate. However, if varicose veins significantly affect quality of life or aesthetics, surgery may be a suitable option. It is advisable for patients to make informed decisions based on individual circumstances under the guidance of a qualified physician. Is surgery for lower limb superficial vein varicosity a permanent solution? Varicose veins have a high tendency to recur, necessitating long-term care post-surgery to maintain favorable outcomes. References: International Vascular Alliance China Branch Nursing Professional Committee, Chinese Medical Doctor Association Interventional Vascular Medicine Professional Committee. Expert consensus on the use of gradient compression stockings in the prevention and treatment of venous thromboembolism. Journal of Interventional Radiology, 2019, 28(9): 811-818. Note: Some images generated by Doubao AI. Note: The cover image is sourced from a copyright stock photo library; unauthorized usage may result in copyright disputes.
© 2025 Health Tribe.