What casual actions are silently harming your eyes?

Author: Li Min from Zhuzhou Eye Hospital. Reviewer: ZS. Production Information: Hunan Medical Communication. Title: What casual actions are silently harming your eyes? Introduction: Keratoconus affects vision; this article highlights its causes, symptoms, and preventive measures for eye health.
In clinical outpatient settings, some children and adolescents may frequently rub their eyes for extended periods without timely professional examinations. This mechanical action may trigger keratoconus, and if the condition continues to progress, corresponding medical intervention may be required.
Keratoconus is a type of chronic, progressive corneal disorder that is relatively common among children and adolescents. Its early symptoms are often atypical and may be easily overlooked, potentially delaying early intervention. The continued progression of the condition can lead to a decrease in corneal thickness and abnormal shape, adversely affecting visual quality.
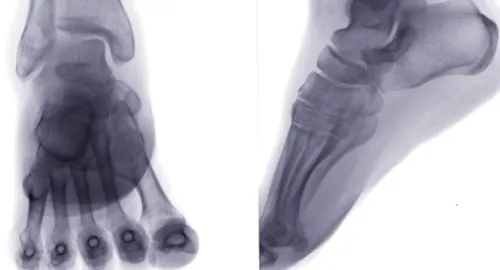
What is keratoconus? Keratoconus is a commonly seen non-inflammatory, chronic, and progressive localized corneal ectasia disease, characterized primarily by corneal expansion and thinning in the central or para-central area, resulting in a conical protrusion. From a lateral view, the corneal shape appears to bulge forward, and such manifestations warrant timely medical examination. The progression of the condition involves gradual corneal expansion and a decrease in thickness, which can lead to significant irregular astigmatism, subsequently affecting vision.
Keratoconus is commonly seen in the adolescent population, with most patients being in their teenage years. Public awareness of the condition is relatively low, and an accurate diagnosis relies on specialized equipment and clinical experience, making early recognition somewhat challenging and often leading to delays in diagnosis. If the disease continues to progress, appropriate intervention measures need to be taken based on the condition of the eyes.
Why does keratoconus occur? The causes of keratoconus are not yet fully understood, but it is currently believed to be related to a reduction in corneal collagen content and abnormal arrangement of collagen fibers, which leads to a decrease in corneal mechanical strength and changes such as thinning and protrusion. Genetic factors and allergic predispositions may also be associated with the onset of the disease. In addition, poor habits such as excessive eye rubbing have been confirmed to potentially trigger this condition.
Daily advice: Try to avoid excessive rubbing of the eyes and reduce sleeping on your stomach to lessen pressure on the eyeballs. If frequent eye rubbing is caused by allergic conjunctivitis, dry eyes, or other eye conditions, it is important to promptly seek proper treatment for the underlying issue.
How to know if you have keratoconus? Experts from Zhuzhou Aier Eye Hospital have indicated that some patients may experience acute corneal edema, accompanied by a sudden decline in vision. Other patients may have a relatively mild progression of the condition, with less significant vision loss, which can easily be confused with simple myopia or astigmatism.
The clinical course of keratoconus can be divided into four stages: 1. Incubation period: The diagnosis is relatively difficult. If one eye has been diagnosed with keratoconus and the opposite eye has refractive errors, it is necessary to remain vigilant and conduct close follow-up. 2. Initial: Routine examinations may show no significant abnormalities, with only the optometry indicating varying degrees of myopia and astigmatism. The corneal topography examination may reveal a slight decrease in corneal thickness and an increase in the height of the posterior surface. 3. Progressive stage: Vision deterioration is quite significant, the corrective effect of framed glasses is not satisfactory, the corneal curvature increases, and there is a noticeable trend of corneal thinning. 4. Severe stage of the disease: The cornea presents with a conical protrusion, the stroma becomes thinner, and some may experience stromal rupture leading to scarring; if the posterior elastic layer ruptures, it may be accompanied by signs of acute corneal edema.
How should keratoconus be intervened? Clinical interventions will be tailored to the stage and progression characteristics of keratoconus. In the early stages, when the condition is stable, vision improvement and visual quality enhancement can be achieved through optical correction methods. If there is a trend of progression, professional interventions can be employed to strengthen the cornea and slow down the progression of the disease. In cases of more severe impairment, ocular repair methods are necessary to improve visual function.
Warm reminder: If there is a significant increase in astigmatism in a short period, accompanied by a noticeable decline in vision, and conventional optical correction is not effective, it is advisable to visit a professional ophthalmology institution for an examination and assessment to understand the condition of the eyes in a timely manner.
Follow @HunanMedicalChat for more health science information! (Edited ZS)
© 2025 Health Tribe.